Our Office
1744 Fry Rd.
Houston, TX 77084
Existing Patients: (281) 492-8900
New Patients: (281) 213-5048
Fax: (281) 492–9337
Email: briterdental1744@gmail.com
Visit Us Online
Bone Grafts: Restoring Jawbone Strength and Facial Support
Bone loss around the jaws can affect chewing, the fit of dental restorations, and the natural contours of the face. Whether the cause is missing teeth, periodontal disease, or trauma, insufficient bone compromises both function and appearance. For many patients considering implants or more stable restorations, rebuilding that lost bone is an essential first step.
At Briter Dental, our approach is to explain the purpose and benefits of grafting clearly so patients can make informed decisions. The procedures we describe here focus on predictable methods for encouraging new bone growth, improving long-term outcomes for implants and other restorative care, and preserving facial structure.
Bone is living tissue that responds to stimulation from teeth and chewing forces. When a tooth is lost, the underlying bone no longer receives the normal mechanical signals that maintain volume. Over time this leads to resorption — the ridge narrows and the vertical height can decline — which can change how your smile and lower face look.
Beyond aesthetics, adequate bone is critical for oral function. Sufficient width and height are required to anchor dental implants securely and to provide predictable support for bridges and overdentures. Restoring bone where it has been lost reduces the risk of complications and expands restorative options.
Bone loss may also be associated with periodontal disease and infections. Addressing the underlying cause in tandem with grafting helps create a healthier environment where new bone can form and integrate with future restorative work.
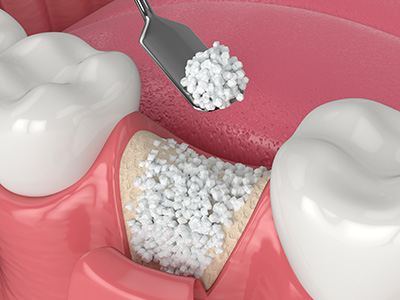
A bone graft provides a framework that encourages the body to form its own bone. Think of graft material as a scaffold that supports the migration of cells and blood vessels essential for new tissue development. Over time the scaffold is replaced by the patient’s own bone, creating a stable foundation for restorations.
Graft materials come from several sources: autografts (the patient’s own bone), allografts (processed donor bone), xenografts (animal-derived materials), and synthetic bone substitutes. Each option has advantages and is chosen based on the patient’s clinical needs, the size of the defect, and anticipated healing.
In many cases clinicians also use barrier membranes or biologically active agents to guide healing and protect the graft while new bone forms. These adjuncts help keep soft tissue out of the graft site and can accelerate or improve the quality of regeneration in certain situations.
Grafts can be placed at different times depending on the clinical scenario. An immediate graft performed at the time of tooth extraction — often called ridge preservation — helps limit the natural shrinking of the socket and preserves tissue for future implant placement. This single-visit approach reduces overall treatment time and preserves more of the original bone shape.
When significant resorption has already occurred, a delayed grafting procedure is usually required. In these cases the surgeon reflects the soft tissue, exposes the bone defect, places the graft material, and closes the site to allow healing. Depending on the extent of augmentation needed, healing may take several months before implants or other restorations are placed.
Choosing the right timing is a matter of balancing immediate preservation with the need for a stable, healthy foundation. A careful clinical and radiographic evaluation helps determine whether an immediate graft, a staged approach, or a combination is best for each patient.
When the upper back jaw lacks sufficient bone height for an implant, a sinus lift is a common solution. In this procedure the sinus membrane is carefully elevated and graft material is placed beneath it to increase vertical bone height. Once healed, the augmented area can support implants that otherwise would not be feasible in that location.
For patients seeking the best restorative or cosmetic result, ridge augmentation techniques are used to rebuild natural contours. These procedures restore volume to areas where the ridge has collapsed, improving the emergence profile for crowns, bridges, or implant restorations and helping achieve a more natural-looking outcome.
Both sinus lifts and aesthetic ridge augmentations rely on precise surgical technique and appropriate graft material selection. In many cases the use of barrier membranes and biologically active products complements the graft and helps achieve predictable, long-lasting results.
Successful grafting begins with a thorough evaluation, including medical history, clinical exam, and three-dimensional imaging when needed. Imaging helps the surgical team assess the size and shape of the defect, plan graft placement, and identify anatomical structures such as the sinus or nerve canals that must be protected.
After the procedure, patients are given clear instructions to support healing: gentle oral hygiene, short-term dietary modifications, and guidance about activity and medications. Healing times vary with the type and size of the graft; while some improvements are felt quickly, complete maturation of new bone often takes several months.
Long-term success depends on good oral hygiene and routine follow-up care. Smoking and certain medical conditions can impair healing, so candid discussion of health habits and realistic expectations is an important part of treatment planning.
In short, bone grafting is a reliable tool for restoring lost jawbone, enabling predictable implant placement, and preserving facial form. If you’d like to learn whether bone grafting is right for you, please contact us for more information and to schedule a consultation with our team at Briter Dental.
A bone graft is a surgical procedure that places material into an area of jawbone loss to encourage new bone formation and restore structural support. The graft acts as a scaffold that native bone cells can grow into, helping to rebuild width or height where bone has been resorbed. This restoration is important for chewing function, long-term dental health, and maintaining the natural contours of the face.
People commonly need bone grafts after tooth loss, periodontal disease, trauma, or when there is inadequate bone to support a dental implant. A graft can be used to preserve the ridge after extraction or to augment a deficient area before or during restorative treatment. Treatment planning usually involves clinical evaluation and imaging to determine the extent of bone loss and the appropriate grafting approach.
When a tooth is removed the stimulation provided by biting and chewing is lost, and the surrounding bone begins to remodel and resorb. Studies show that significant ridge width can be lost within the first year after extraction, which can compromise future restorative options and alter facial support. Placing a graft at the time of extraction helps reduce this resorption and preserves the dimensions needed for later treatment.
Immediate grafting at extraction produces a more predictable ridge for future implant placement or prosthetic work compared with allowing the site to heal without intervention. When a graft is delayed, a second surgical procedure is required to expose the bone and place graft material, which can lengthen treatment time. Your clinician will weigh the benefits of immediate preservation against clinical factors such as infection, tissue health, and overall treatment goals at Briter Dental.
Graft materials commonly include autografts (bone taken from the patient), allografts (processed human donor bone), xenografts (derived from animal sources), and alloplasts (synthetic bone-like materials). Each option has distinct biological properties: autografts are osteogenic and integrate well, while allografts and xenografts are osteoconductive scaffolds that support new bone growth. Synthetic materials can provide predictable volume and avoid donor-site morbidity, and are often used when small augmentations are needed or when patient preference favors non‑biologic options.
The choice of graft material depends on the defect size, location, patient medical history, and the clinician’s goals for healing and integration. In many cases, combinations of materials and biologically active adjuncts are used to optimize outcomes. Your surgeon will explain the advantages and trade-offs of each option and recommend a material based on evidence and the specifics of your case.
A sinus lift, also called a sinus augmentation, is a specific grafting procedure performed to increase bone height in the upper posterior jaw where the maxillary sinus is close to the alveolar ridge. The surgeon elevates the sinus membrane and places graft material between the jawbone and the sinus floor to create sufficient vertical bone for implant placement. This procedure is indicated when routine implant placement would encroach on the sinus or when there is inadequate bone height due to long-term tooth loss or anatomic variation.
Sinus lifts are planned using diagnostic imaging to measure the available bone and assess sinus anatomy, and they can be performed as a staged procedure or simultaneously with implant placement depending on the remaining bone height. Healing timelines vary, and the clinician monitors integration with follow-up imaging before proceeding with implant placement. Meticulous technique and careful handling of the sinus membrane help minimize complications and improve graft success.
Bone grafting can be performed under local anesthesia with or without sedation depending on the complexity of the case and patient comfort needs. For immediate grafts the tooth extraction and graft placement occur during the same visit; for delayed grafts the surgeon reflects the soft tissue to expose the defect, places the graft material, and secures it before closing the tissues. In many cases, protective membranes or biologically active materials are placed over the graft to guide tissue regeneration and stabilize the graft during healing.
Procedures typically take from less than an hour for small ridge preservation grafts to longer for larger augmentations or sinus lifts, and you will receive detailed post-operative instructions to support healing. Pain control, infection prevention, and activity limitations are discussed beforehand to set expectations. Follow-up visits allow the team to evaluate healing and plan any subsequent restorative steps such as implant placement.
After a bone graft most patients experience normal post-operative symptoms such as swelling, mild to moderate discomfort, and some bruising that peak in the first 48 to 72 hours. The surgeon will recommend pain control measures, cold compresses initially, and specific oral hygiene instructions to protect the surgical site while supporting healing. Avoiding smoking, strenuous activity, and actions that increase sinus pressure helps reduce the risk of complications and supports graft integration.
Diet is typically soft for several days, and you will return for follow-up appointments so the clinician can monitor tissue healing and, if used, remove sutures according to the chosen technique. If any signs of infection, persistent bleeding, or unexpected pain occur, contact the office promptly for evaluation. Adhering to post-operative directions and attending scheduled visits are important for the best possible outcome.
Healing times vary with the type and size of the graft, the graft material used, and the location in the jaw, but a common range for graft maturation before implant placement is three to six months. Smaller ridge preservation grafts often integrate more quickly, while larger augmentations and sinus lifts may require longer healing periods to achieve sufficient bone quality. Clinicians use clinical evaluation and imaging to confirm that the graft has consolidated and can support an implant.
In some cases, implants can be placed simultaneously with grafting if primary stability is achievable and the remaining bone is adequate. In other situations a staged approach is safer and more predictable, allowing the graft to mature completely before implant surgery. Your dental team will recommend the timing that balances predictability, biology, and your overall treatment plan.
As with any surgical procedure, bone grafting carries risks that may include infection, graft exposure or failure, bleeding, and delayed healing; specific procedures such as sinus lifts also carry the risk of sinus membrane perforation. Smoking, uncontrolled systemic conditions, and poor oral hygiene can increase the likelihood of complications or compromise graft integration. Careful patient selection, sterile technique, and thorough preoperative assessment help reduce these risks.
When complications occur they are usually manageable with prompt care such as antibiotics, local wound management, or revision procedures if necessary. Your surgeon will discuss potential risks during the consultation and explain how medical history, medications, and lifestyle factors can influence outcomes. Open communication and adherence to post-operative instructions are key to minimizing problems and promoting successful healing.
Bone provides foundational support for the overlying soft tissues and lips, so loss of bone can lead to flattening of facial contours, changes in lip support, and a prematurely aged appearance in the affected area. Ridge augmentation restores lost bone volume and contour, which improves the support for gum tissue and prosthetic restorations and contributes to a more natural, balanced facial profile. These aesthetic benefits are often important when planning crowns, bridges, or implant-supported restorations in the visible smile zone.
An aesthetic ridge augmentation focuses not only on creating adequate bone for function but also on sculpting a pleasing contour that harmonizes with adjacent teeth and soft tissue. The procedure may be combined with soft tissue management to optimize the final cosmetic outcome, and the treatment plan is tailored to the patient's anatomic needs and aesthetic goals. Discussing expectations and visual goals with your clinician helps achieve a result that is both functional and attractive.
The best way to determine if a bone graft is appropriate is to schedule a consultation that includes a thorough clinical exam and diagnostic imaging such as panoramic or cone beam CT scans to assess bone volume and anatomy. During the visit the surgical or restorative team will review your dental history, overall health, and treatment goals to develop a personalized plan that outlines recommended procedures and timelines. This comprehensive evaluation helps identify whether immediate preservation, staged augmentation, or alternative approaches are most suitable for your case.
At a consultation you can also discuss graft material options, potential risks, and the sequence of restorative steps that follow grafting, including implant placement if that is your goal. The team will explain follow-up care, expected healing times, and signs to watch for during recovery so you have a clear understanding of the process. If you are located in Katy, Texas, our staff can arrange an appointment and provide any additional information needed to prepare for the evaluation.